Preventing heart disease using augmented digital health intelligence
12 January 2022 / 10:01 am
Coronary heart disease remains one of the biggest killers in Western society and it is estimated that there are 7.6 million people living with heart and circulatory disease in the United Kingdom (1). Every five minutes someone is admitted to hospital in the UK with a heart attack. Many people however have heart disease without being aware that there is anything wrong, and half of heart attack patients have no symptoms or warning before their event.
Coronary heart disease is caused by an inflammatory process – where inflammation in the wall of the heart arteries allows the build-up of fatty deposits in the arteries called plaques. If these plaques block the flow of blood in the artery, then this can result in symptoms such as chest pain on effort or angina. If the plaque ruptures, then a blood clot can suddenly reduce the flow of blood further resulting in a heart attack or sudden cardiac death.
It is estimated that 90% of premature heart disease is preventable. Traditional behavioural measures are extremely effective at preventing disease and heart attacks, such as cessation of smoking, weight loss, and exercise, as well as the introduction of medicines to control blood pressure, diabetes, and cholesterol (2). Interventional procedures such as coronary stents and bypass surgery can help in selected individuals. There are new pharmaceutical agents available such as the PCSK9 inhibitors Evolocumab and Alirocumab, and the small interfering RNA (siRNA) molecule Incliseran. There are also increasing data on the use of anti-inflammatory drugs such as colchicine to reduce cardiovascular risk.
In patients with no symptoms there are different ways of assessing the risk of having or developing coronary heart disease. One of the most commonly used systems is called QRisk https://qrisk.org/three and calculates a person’s risk of developing a heart attack or stroke over the next ten years. This traditionally categorises people into low, intermediate and high-risk groups. People in low-risk groups are reassured, people in intermediate-risk groups given advice to lower their risk and people in high-risk groups started on medicines.
Until recently we haven’t been able to measure the inflammation in the heart arteries but, thanks to a new digital health technology provided by Caristo www.caristo.com we are now able to quicky and accurately assess it (3).
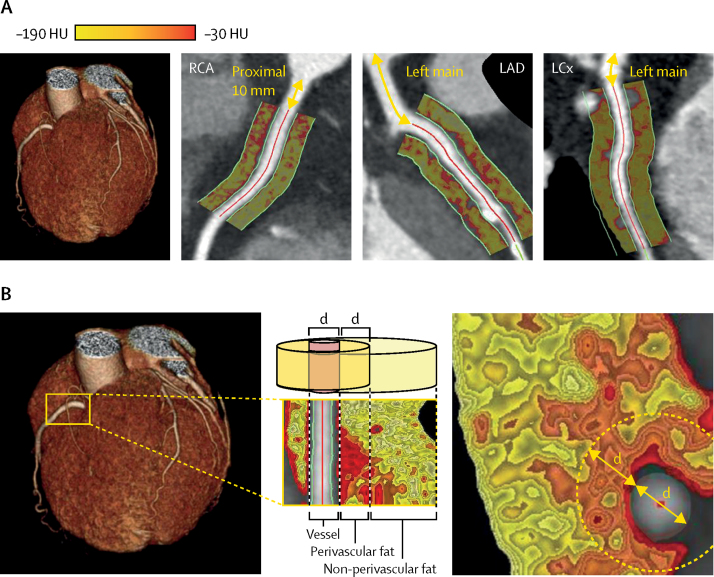
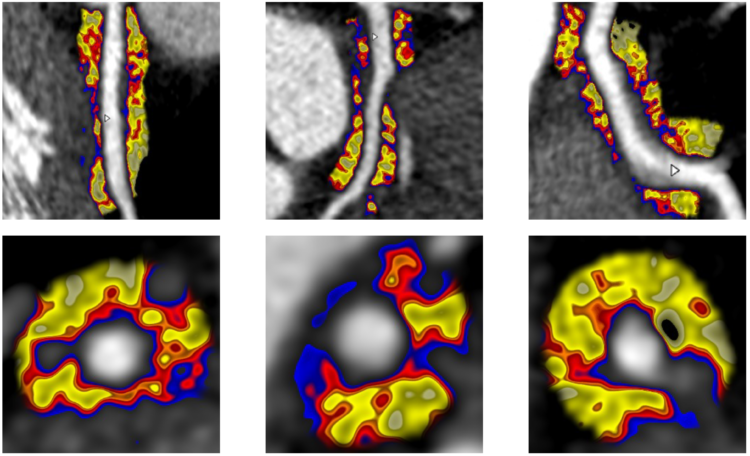
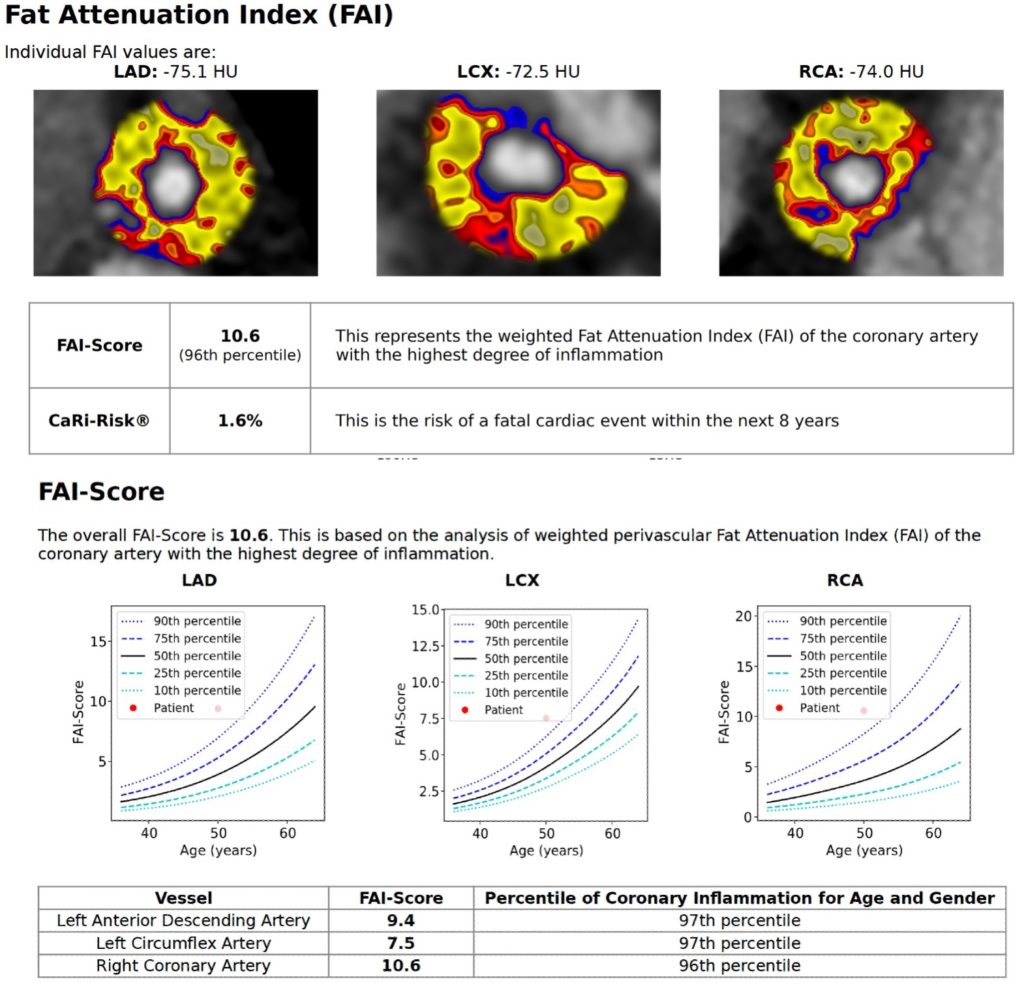
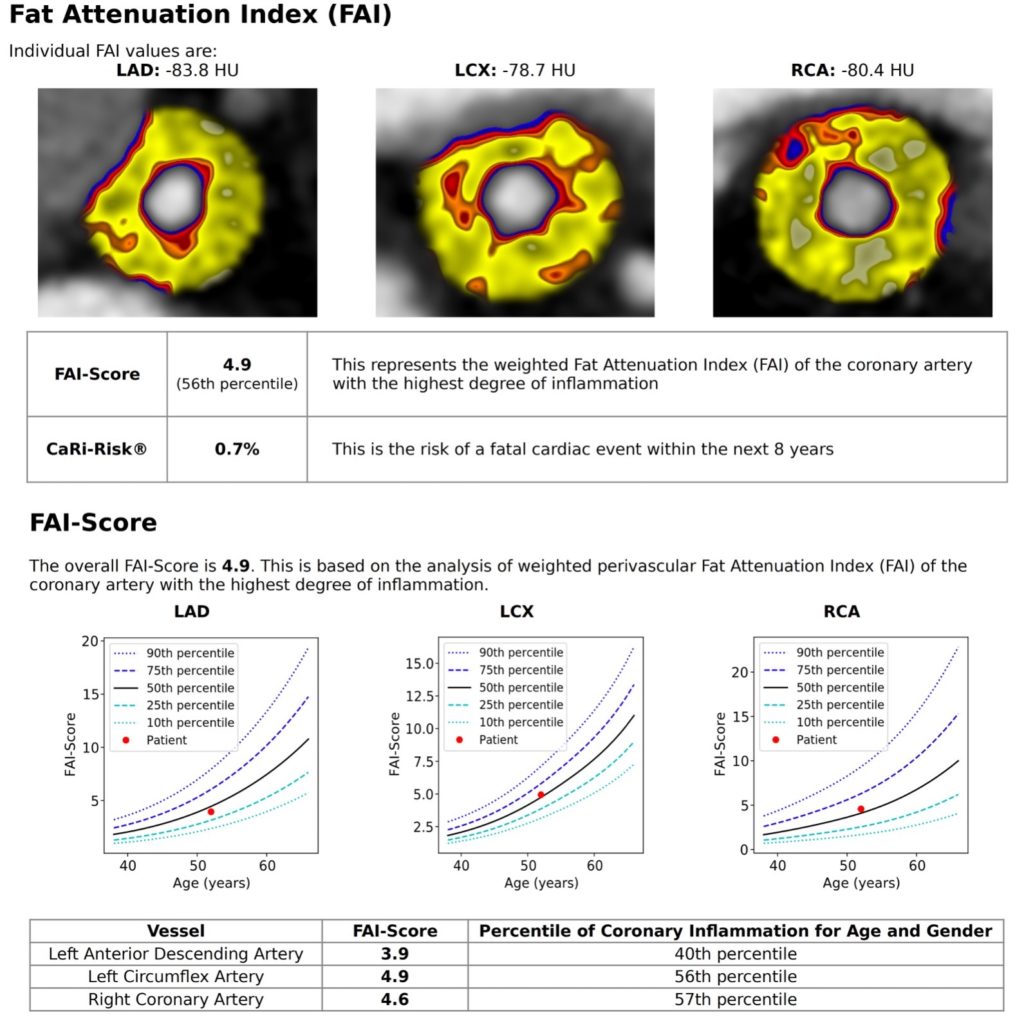
In order to have the test, patients first have a CT coronary angiogram to look at their heart arteries and then the images are analysed using an artificial intelligence algorithm to assess the Fat Attenuation Index (FAI).
When the CT images are combined with traditional risk factors this provides the absolute risk of a fatal cardiac event within the next eight years – the CaRi-Heart® risk. This score significantly improves risk discrimination over clinical risk factor-based models such as QRisk and reclassifies about a third of the population more accurately. This augmented intelligence can then guide individual treatment decisions such as outlined below (4).
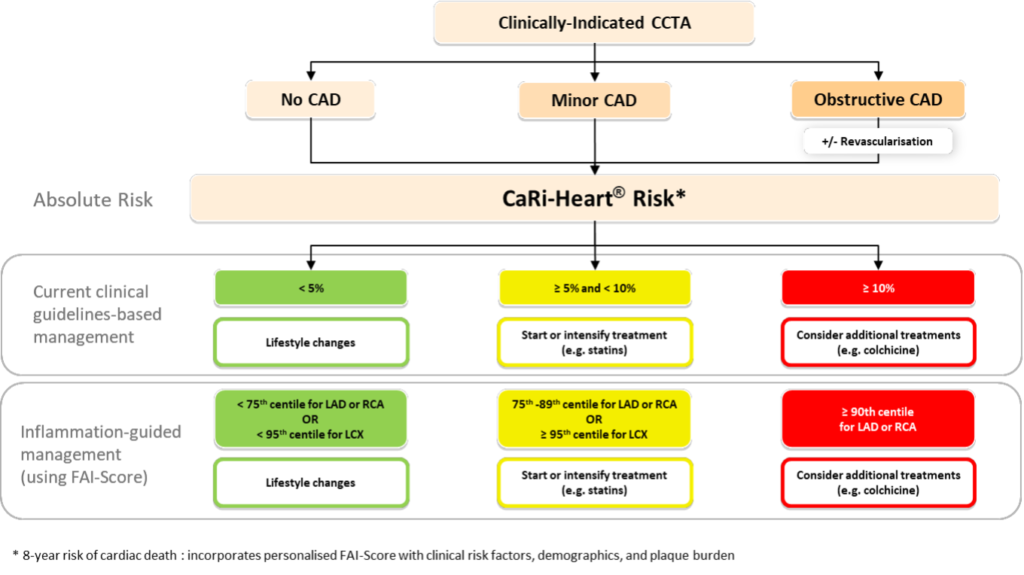
In practice the use of FAI-Score CaRi-Risk® can lead to changes in clinical practice as indicated in these case examples, presented with patient permission.
Case example 1
A 50-year-old man with a family history of heart disease and high cholesterol attended for an assessment of his vascular risk. He was already taking a statin and had no symptoms. He had a normal CT coronary angiogram but his FAI-Score was elevated at the 96th percentile putting him at increased risk of future events. As a consequence, his dose of statin was doubled, and he has entered a preventative surveillance programme.
Case example 2
A 52-year-old man with known coronary heart disease attended for further imaging to assess his future cardiac risk. His FAI-Score was about average predicted and his CaRi-Risk® was low so the patient was reassured, and his medication was continued, unchanged.
Conclusions
FAI and the CaRi-Heart® risk provide valuable personalised risk data that supersedes historic assessments such as CT cardiac calcium scores. We now have the tools to accurately inform patients of the condition of their coronary arteries as well as using the augmented intelligence provided by Caristo to calculate the risk of dying from heart disease. The scores will also help guide the use of the novel (and expensive) PCSK9 modifying medicines providing targeting drug therapy to those at highest risk.
Thanks to the works of our digital health delivery teams HealthX and the Allan Lab we are pleased to say that Jersey is one of the first places in the British Isles to provide this risk assessment using Caristo. For more information on how to have this done please contact Dr Andrew Mitchell via his website.
References
- British Heart Foundation Statistics 2021 https://www.bhf.org.uk/what-we-do/our-research/heart-statistics
- 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. European Heart Journal 2021;42:3227-3337 https://doi.org/10.1093/eurheartj/ehab484
- Non-invasive detection of coronary inflammation using computed tomography and prediction of residual cardiovascular risk (the CRISP CT study): a post-hoc analysis of prospective outcome data. Lancet 2018; 392: 929–39 https://doi.org/10.1016/S0140-6736(18)31114-0
- Standardized measurement of coronary inflammation using cardiovascular computed tomography: integration in clinical care as a prognostic medical device. Cardiovascular Research 2021;117:2677–2690 https://doi.org/10.1093/cvr/cvab286
Links
British Heart Foundation www.bhf.org.uk
Caristo www.caristo.com
The Allan Lab www.theallanlab.com
Dr Andrew Mitchell www.jerseycardiologist.com
More Posts
7 May 2025
A digital health diary revisited
16 March 2024
Developing a new strategy for healthy Islanders
4 February 2024
A digital health diary for Jersey
27 December 2022
Utilising artificial intelligence in cardiology practice
12 June 2022
Under the bonnet – time for your heart’s MOT
12 March 2022
What is heart valve disease and what does that mean for me?
1 October 2021
How heart health has been impacted by COVID-19
1 August 2021
The importance of the rhythm of your heart
21 June 2020
What is atrial fibrillation?
8 April 2020
Coronary heart disease and risk of heart attacks
11 January 2020
The Era of Immersive Health Technology
22 September 2019
The heart and stress
18 August 2019
Screening for Atrial Fibrillation and the Role of Digital Health Technologies
20 November 2018
Ectopic beats – how many count?
28 July 2018
How can immersive VR and AR technologies improve your physical and mental health?